Ulcerative Colitis: A Comprehensive Guide
Introduction
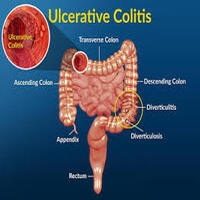
Ulcerative Colitis (UC) is a chronic inflammatory bowel disease (IBD) that affects the large intestine (colon) and rectum. It causes inflammation and ulcers on the inner lining of the colon, leading to discomfort and digestive issues. Unlike other digestive disorders, UC is a long-term condition that can have a significant impact on a person’s quality of life. This article explores the causes, symptoms, diagnosis, treatment options, and lifestyle changes that can help manage ulcerative colitis.
What is Ulcerative Colitis?
Ulcerative colitis is an autoimmune disease, meaning the body’s immune system mistakenly attacks healthy tissues in the colon. This causes inflammation and tiny sores, or ulcers, on the lining of the colon, leading to symptoms such as diarrhea, abdominal pain, and rectal bleeding. UC usually begins gradually and can worsen over time. Although there is no known cure, proper treatment and lifestyle changes can help manage the symptoms and achieve long-term remission.
Types of Ulcerative Colitis
There are several types of ulcerative colitis, classified based on the location and severity of inflammation:
- Ulcerative Proctitis: Inflammation is limited to the rectum. Symptoms are often mild and may include rectal bleeding and urgency.
- Proctosigmoiditis: Inflammation affects the rectum and lower end of the colon (sigmoid colon). Symptoms include abdominal cramps, bloody diarrhea, and pain.
- Left-sided Colitis: Inflammation extends from the rectum up through the descending colon. Symptoms include weight loss, bloody diarrhea, and severe pain on the left side of the abdomen.
- Pancolitis: This type affects the entire colon and can cause severe symptoms, including fatigue, significant weight loss, and severe abdominal pain.
- Acute Severe Ulcerative Colitis: A rare and serious form of UC that affects the entire colon, leading to intense pain, heavy bleeding, and fever. It requires immediate medical attention.
Causes and Risk Factors
The exact cause of ulcerative colitis is unknown, but it is believed to involve a combination of genetic, environmental, and immune system factors:
- Genetics: People with a family history of UC are at a higher risk of developing the condition.
- Immune System Malfunction: An abnormal immune response may cause the body to attack the cells in the digestive tract.
- Environmental Factors: Certain environmental triggers, such as diet and stress, may worsen symptoms.
- Age and Ethnicity: UC can occur at any age but is commonly diagnosed between ages 15 and 30. It is more common in Caucasians and Ashkenazi Jews.
- Lifestyle Factors: A high-fat diet, smoking, and excessive antibiotic use may increase the risk.
Symptoms of Ulcerative Colitis
Symptoms vary depending on the severity and location of inflammation. Common symptoms include:
- Diarrhea with Blood or Pus: Frequent, urgent bowel movements with blood or mucus.
- Abdominal Pain and Cramping: Often felt on the left side of the abdomen.
- Rectal Pain and Bleeding: Pain during bowel movements and bright red blood in the stool.
- Fatigue and Weakness: Due to loss of blood and nutrients.
- Weight Loss and Loss of Appetite: Caused by malabsorption of nutrients and decreased appetite.
- Fever: Especially during severe flare-ups.
Other symptoms can include joint pain, skin issues, and eye inflammation.
Diagnosis of Ulcerative Colitis
Diagnosing ulcerative colitis involves a combination of medical history, physical examination, and diagnostic tests:
- Blood Tests: To check for anemia (low red blood cells) and signs of inflammation.
- Stool Tests: To rule out infections and detect blood in the stool.
- Colonoscopy: A detailed examination of the colon using a flexible tube with a camera. Biopsies may be taken for laboratory analysis.
- Flexible Sigmoidoscopy: Examines the lower part of the colon.
- Imaging Tests: X-rays, CT scans, and MRI can help visualize inflammation and complications.
- Endoscopy: Used in some cases to examine the upper digestive tract.
Treatment Options
There is no cure for ulcerative colitis, but several treatments can help manage symptoms and achieve remission:
- Medications:
- Aminosalicylates (5-ASA): Anti-inflammatory drugs to reduce inflammation in the colon.
- Corticosteroids: Used for short-term flare-ups to reduce inflammation.
- Immunomodulators: Suppress the immune system to prevent inflammation.
- Biologics: Target specific proteins in the immune system to reduce inflammation.
- JAK Inhibitors: Block specific enzymes linked to inflammation.
- Antibiotics: Used to treat or prevent infections.
- Surgery:
- Proctocolectomy: Removal of the colon and rectum, followed by the creation of an ileostomy (an opening in the abdomen for waste elimination).
- Ileoanal Pouch Surgery: After removing the colon, a pouch is created from the small intestine, allowing for more natural bowel movements.
- Diet and Lifestyle Changes:
- Eating smaller, more frequent meals.
- Avoiding trigger foods such as spicy foods, dairy, caffeine, and high-fiber foods.
- Staying hydrated to prevent dehydration from diarrhea.
- Managing stress through relaxation techniques like yoga and meditation.
- Alternative Therapies:
- Probiotics to support gut health.
- Omega-3 supplements for anti-inflammatory effects.
- Acupuncture and herbal remedies (under medical supervision).
Complications of Ulcerative Colitis
If not managed properly, ulcerative colitis can lead to several complications, including:
- Severe Dehydration: Due to frequent diarrhea.
- Colon Cancer: Long-term inflammation increases the risk of colon cancer.
- Bone Loss (Osteoporosis): Due to steroid use and nutrient malabsorption.
- Toxic Megacolon: A rare but life-threatening condition where the colon rapidly swells.
- Liver Disease: Including primary sclerosing cholangitis.
- Blood Clots: Increased risk of blood clots in veins and arteries.
Regular check-ups and colonoscopies are recommended to monitor and prevent complications.
Living with Ulcerative Colitis
Living with UC requires ongoing management and lifestyle adjustments. Here are some tips:
- Follow a Treatment Plan: Take medications as prescribed and attend regular check-ups.
- Maintain a Balanced Diet: Work with a nutritionist to create a diet that avoids trigger foods while ensuring nutrient intake.
- Stay Hydrated: Drink plenty of water, especially during flare-ups.
- Manage Stress: Practice mindfulness, yoga, or other relaxation techniques.
- Stay Active: Light exercise can help reduce stress and improve overall health.
- Join Support Groups: Connecting with others who have UC can provide emotional support and coping strategies.
Conclusion
Ulcerative colitis is a chronic condition that requires careful management. While there is no cure, effective treatments and lifestyle changes can help individuals live fulfilling lives. Early diagnosis and personalized treatment plans are essential for achieving long-term remission and minimizing complications. If you experience persistent digestive symptoms, consult a healthcare professional for proper evaluation and management.
Final Thoughts
Living with ulcerative colitis can be challenging, but with the right care and support, individuals can lead active, healthy lives. It’s important to stay informed, communicate openly with healthcare providers, and take proactive steps to manage the condition. With ongoing research and advancements in treatment, the future looks promising for those living with UC.